Death in the practice or competition arena is a tragic and rare occurrence in sport. However, while the rate of incidence is low, it’s enough of a concern that screening and education must be implemented to address athlete health and well-being. Sudden cardiac death (SCD) in sport can happen to any athlete at any time, and the risks, while low, are real. In addition to cardiac events, having a contingency plan is essential for all traumatic injuries, as a solid action plan is valuable even for other occurrences that are less severe in nature. Over the last decade, there have been major advancements in screening and diagnosing athlete pathologies that can contribute to SCD and other cardiovascular events. In this Academy Guide, we cover the important areas of risk awareness, screening, management, and monitoring athletes.
A Risk Outlook of Sudden Cardiac Death
Because the risk of SCD is less than 1% of all participating athletes, including older recreational populations, not as much attention is paid to the problem as to traumatic brain injury or other head and neck trauma. SCD is also associated with heat illness and dehydration, but it should be known that the pathologies that place athletes at risk are separate from environmental conditions, and much of risk is genetic. Additional variables like training load and program design are secondary in the risks for SCD, and are only effective in managing athletes who can fully participate in sports.
Due to the low incidence rate, the long-term prognosis for and changes in truly at-risk athletes are unknown. Professional athletes with hypertrophic cardiomyopathy or other abnormalities represent a very small percentage of the population, but due to the increasing interest and larger population of older athletes in recreational sport, SCD risk is rising. Based on demographic information, male athletes who participate in basketball are more at risk than other groups. Female athletes and other sports are less at risk, but all athletes should be screened from both a legal and ethical standpoint.
Cardiac Screening of the Athlete
Many health organizations recommend youth and masters screening, as those populations are at risk and have poor track records of being evaluated for SCD. Other international organizations do not agree on screening athletes, due to the lack of quality randomly controlled studies and the large number of false positives. Elite sport, ranging from college to professional levels, is typically interested in the risk of SCD.
Since the financial consequences and legal ramifications are real, the expectations of care are higher. The cost of a screening may be prohibitive for lower-income families, but as the technology gets better and awareness grows, we will likely see progress in the coming years. Professionals with access to both medical expertise and professional-grade equipment should screen athletes when possible. As of today, there is not enough evidence that simply reporting symptoms and conducting physicals adequately screens for SCD.
SCD assessment and other heart performance evaluations are extensive processes that require both expertise and repeated testing. As mentioned earlier in the conditioning testing guide, electrocardiograms (ECG) can be added to lab testing. Expert cardiologists with experience in sports and exercise are needed to fully diagnose a pathology, and other less dangerous pathologies can be screened concurrently during the evaluations. Other pathologies that are abnormal but still benign are usually found as a possible differential diagnosis. It’s up to the specialist to render a diagnosis and create a plan of care. While the instrumentation is important, the use of ECG has not been proven effective in reducing the death rate of athletes.
After the screening is performed, follow-up testing is still recommended. It’s likely that athletes who have comprehensive assessments using complete screening with ECG, echocardiogram, stress tests, and other evaluations will not need the extensive process repeated annually. Those with false positives usually have follow-up testing to confirm the error and then can move on to routine annual evaluations. Those with a legitimate risk are managed on an individual basis. You should know that no screening system is perfect and it is not currently possible to successfully screen out all at-risk athletes. The current debate over whether screening programs for SCD actually save lives exists because of the lack of quality studies.
Diagnosis of Cardiac Pathologies
Like orthopedic and brain injuries, cardiac pathologies require expertise and a full clinical examination beyond imaging or similar. With false positives common with athletes, there will likely be multiple opinions used to make a diagnosis, as screening is an imperfect process and mistakes in interpreting the available data do occur. If a diagnosis does recommend retirement, the continued participation of the athlete is often a political and legal challenge as the medical evidence is usually seen as expert opinion, unless the pathology is severe.
Finally, the prognosis of a cardiac pathology extends beyond sport and is considered a health risk, thus care must extend beyond the diagnosis and into the treatment and management phase. If athletes have permanent or congenital abnormalities that are with them for their lifetime and require early retirement or cessation of participation in sport, it’s important to include psychotherapy with an expertise in sport. This is because the unexpected findings may cause depression, and coping strategies during the transition should be developed and monitored by professionals.
Management Opportunities for Medical and Performance Staff
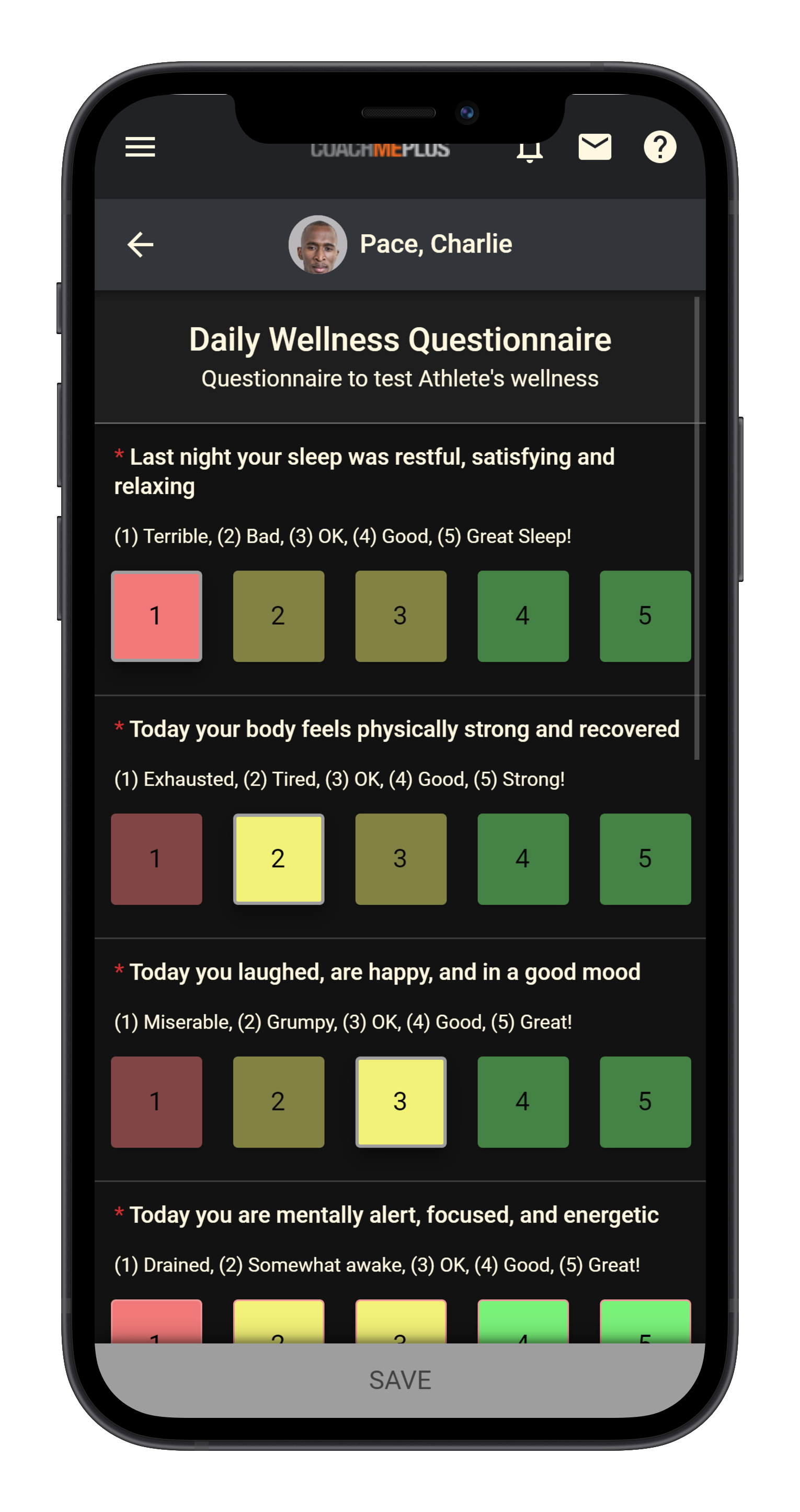
When athletes are faced with a heart condition, regardless of its severity, the first step is education and psychological support. Not providing or not appropriately handling emotional and professional support can lead to anxiety and confidence issues that could reduce performance and quality of life. Thus, a focus on comprehensive holistic care is recommended for the entire staff if an athlete is diagnosed with a heart condition. Implementation of simple daily wellness questionnaires can serve this purpose well.
It may be necessary to outsource to specialists to complete the necessary rehabilitation if treatment is an option. Not all heart pathologies are permanent risks, and some are treatable with specialist care and expert rehabilitation. Transient heart conditions with athletes may need surgery, medications, and cardiac rehabilitation. In addition to the conventional needs of the athlete, a trained sport psychologist is recommended to handle the common fears over participating in high exertion activities. Therefore, an integrated program is suggested with all levels, not just elite programs. Athlete consulting, group therapy, and coach education may be necessary for special cases, as a heart condition is a complex issue faced by teams. Teammates and others involved with the athlete may need to be included.
After successful reintegration into full competition and training, the process may require follow-up checkups and routine screening. Athletes may psychologically feel like they have closure with clearance testing, thus the delicate balance between medical best practices and the psychological realities of athletes is a real challenge. How to handle this dilemma is subject to debate, but medical expertise should drive the appropriate management of discharging athletes when they complete their treatment. Those with ongoing heart conditions should be managed over an entire career so they know their limitations and maintain their health and wellness after sport with confidence.
Monitoring the At-Risk Athlete
At-risk athletes range from those with very low cardiovascular needs to higher risk athletes who may be borderline candidates for early retirement. Due to the large number of individual considerations, a blanket recommendation beyond following the guidelines and protocols of medical professionals is not available in this section. What is important is that a modern sport science program can be complementary to the experienced cardiologist, and supportive monitoring adds more context and validity to the process.
Those who are at risk should follow the exact protocols and recommendations of the specialists, and monitoring the responses to training or rehabilitation requires a focus on clinical symptoms as well as physiological data. The return to play of athletes with pathologies ranges from a brief period of reduced participation to extensive layoffs from competition. At times that risk is deemed life-threatening, retirement is sometimes recommended. Drug interaction and other variables are often monitored, including typical workload and recovery indices all related to athlete surveillance.

Sudden Cardiac Death Challenges and Solutions
A major challenge today is the low occurrence of pathologies that place athletes in jeopardy, so resources such as time and budgets are likely to be applied to other areas, such as concussions and orthopedic injuries. Therefore, staff should look to inexpensive and practical ways to screen, as it is worth employing in conjunction with conditioning tests and general wellness examinations. The probability of a true career-ending pathology is very small, but the process of administering assessments offers a great insight into the morphological adaptations and training effects over time. Therefore, screening is potentially advantageous to teams and organizations wanting to model performance more effectively. Screening and athlete education, as well as careful management of those at risk, are essential to save lives and develop better performance in the long run.

CoachMePlus is a comprehensive solution for any training environment, ranging from scholastic level to pros, and including both military and private facilities.

Recent Comments